Our healthcare system is facing unprecedented challenges with the recent pandemic of coronavirus and ensuing SARS Cov2, or COVID-19, and it is vital healthcare providers keep their patients active and healthy so as to not over burden a vulnerable system.

As an Acute Care Nurse Practitioner researching and practicing advanced endocrinology concepts over the past 12 years, I have recognized an overarching theme: hormones are active and play a vital role in every single body system. The far-reaching impact of restoring hormone homeostasis on health-related quality of life is an often-misunderstood phenomenon in both the healthcare and lay communities.
With the additional burden of stress these uncertain times adds to an already encumbered psyche, classifying hormone therapies as inessential will have dire consequences. This article will outline the vital role hormone homeostasis plays in several common acute and chronic health conditions, dispelling any misconception that hormone maintenance is elective and unnecessary.
Hormones aren’t just for hot flashes and ED
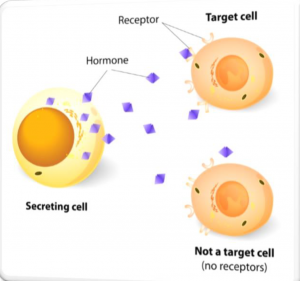
A myth our healthcare providers must often unravel is the concept that hormone therapy (HT) for women is used simply to abate hot flashes, vaginal dryness, and other nasty symptoms of hormone fluctuations; and testosterone replacement therapy (TRT) in men is primarily to assist in sexual function. Nothing could be further from the truth. In fact, these “side effects” of HT and TRT are what we call a bonus. Hormones play a vital role in all body systems. Androgen receptors are found in virtually every tissue in both women and men from the brain, breast, heart and bones, indicating the role they play in normal tissue homeostasis as well as pathologies such as breast cancer, osteoporosis, neuropsychological and neuro-cognitive decline as well as cardiovascular and a plethora of other disease processes 1.
In addition to improving overall sense of well-being, energy levels, libido and quality of life (QOL), HT has been shown to prevent osteoporosis, reduce cardiovascular disease risk, reduce hypertension, increase muscle mass, increase muscle strength, increase bone density, reduce visceral fat, reduce total cholesterol levels, induce glucose homeostasis, increase metabolism, manage PMS, reduce severity and frequency of migraine headaches, improve cognition,
improve memory, prevent Alzheimer’s disease, and improve Parkinson’s symptoms, thus having a positive impact on health related QOL 2.
1. Aminorroaya, et. al., 2005; Amory, et. al., 2004; Araujo, et. al., 2011; Bachmann, 1999; Beauchet, 2006; Bialek, et. al., 2004; Boyanov, et. al., 2003; Cherrier, et. al.,
2001; Davis, 1999; Davis & Tran, 2001; Davison, et. al., 2011; Glaser, et. al., 2012; Hammond, et. al., 2001; Isidori, et. al., 2005; Okun, 2006; Pike, et. al., 2009;
Vanderschueren, et. al., 2004; van Geel, 2009
2. Bachmann, 1999; Conner, et. al., 2008; Carnahan & Perry, 2004; Davis, et. al., 2001; Davis & Tran, 1999; Dokovic, et.al., 2015; Ebinger, et. al., 2008; Frye, et.al., 2009;
Glaser, et.al., 2011; Glaser, et.al., 2013; Glaser & Dimitrikakis, 2013; Hodosy, et.al., 2012; McHenry, et.al., 2014; Miller, et.al., 2007; Miller, et.al., 2009; Nappi &
Lachowsky, 2009; Osborne, et.al., 2009; Panay & Fenton, 2009; Sands & Studd, 1995; Schutter, et.al., 2005; Studd & Panay, 2004; Zarrouf, et.al, 2009

Psychological
Androgen and estrogen replacement have been shown improve mood, lift anxiety and depression, and improve sleep patterns. The hippocampus and amygdala, critical regions in the brain owing to incidence of depression, are rich with androgen receptors, a key explanation of clinical response with androgen therapy 3. Sleep deprivation has the most significant compounding effect and exacerbates the depression, anxiety, moodiness and impaired cognitive function a person may be experiencing with absent or sub optimal hormones. The presence of depression, anxiety and altered mood states is a widespread, worldwide phenomenon, crossing cultural and ethnic lines 4. Depression and anxiety are twice as likely to occur in women as in men, are a leading cause of dysfunction and disability in women and noted in several studies to be a key component of decreased QOL and sense of well-being 5.
The differences between men and women in depression rates have also been observed worldwide, and these documented sex differences have led to the scholarly observation that hormone fluctuations are a major contributor 6. Depression in men is an often-overlooked diagnosis, and men with sub optimal testosterone are more than twice as likely to suffer mental health issues than their optimized counterparts 7.
Cardiovascular Disease
Cardiovascular disease is of utmost concern with regards to an overburdened healthcare system. Heart disease rates and heart attacks have soared in recent years, despite the judicious use of statins. Hundreds of studies reveal the essential role sex hormones play in cardiovascular disease prevention and stabilization. Further, many recent studies have demonstrated the detrimental effects of discontinuing hormone therapy in women. A landmark study reviewed the number of excess deaths from avoidance of HT, namely estrogen. This study came on the heels of HT avoidance post publication of the Women’s Health Initiative (WHI) trial when the media portrayed “hormones” as bad for women. Providers stopped prescribing based on misinterpretation of the WHI data by the media, and the results revealed a staggering 91,610 excess, avoidable, deaths in women who had had a hysterectomy and not been given HT to manage the deficiencies 8. The number did NOT include women globally with hormone decline who had not had a hysterectomy.
3. Ebinger, et.al., 2008
4. Ebinger, et.al., 2008; Gyllstrom, et.al, 2007
3. Davis & Tran, 2001; Gyllstrom, et.al., 2007; McHenry, et.al., 2014; Rohr, 2002
5. Gyllstrom, et.al, 2007, Bromberger, et.al., 2007;
6. Freeman, et.al., 2004; Maartens, et.al., 2002; Panay & Fenton, 2009; Soares, et.al., 2003; 6. Studd & Panay, 2004
7. Jung & Shin, 2016;
8. Gagliano, et.al., 2018; Sarrel, et.al., 2013
Other studies revealed discontinuing estrogen in women was associated with increased risk of cardiac and stroke death in the first post treatment year. Rapid withdrawal of estrogen and discontinuation of HT may result in vasoconstriction and potentially adverse arterial changes and cardiovascular events, as the vasodilatory effects of estrogen suddenly cease.
Declining estrogen may also modulate cardiac rhythm, perhaps via calcium ion channels or by preventing long QT interval. Acute withdrawal of estrogen may predispose to fatal arrhythmia’s.
Increased cardiovascular death risks question the safety of HT discontinuation practice to evaluate whether a woman could manage without HT. Further, women who stayed on their HT had a vastly reduced mortality rate compared with women who stopped treatment 9.
Low serum testosterone is associated with several cardiovascular risk factors including dyslipidemia, adverse clotting profiles, obesity, and insulin resistance. Testosterone has been reported to improve symptoms of angina and delay time to ischemic threshold in unselected men with coronary disease. In men, endogenous testosterone concentrations are inversely related to mortality due to cardiovascular disease and all causes. Low testosterone may be a predictive marker for those at high risk of cardiovascular disease, and Low testosterone is an independent predictor of severity of CAD 10.
Androgenic hormones are beneficial for endothelial cells (ECs) because these hormones induce nitric oxide production, proliferation, motility, and growth of ECs; inhibit inflammatory activation and induction of procoagulant, and adhesive properties in ECs. Further, androgens show anti-thrombotic properties, thereby possessing cardioprotective function 11. One study showed a strong and independent association between low serum (blood) concentrations of testosterone and heart attacks in men with type 2 diabetes 12.
Low testosterone is associated with hypertension in several studies. Molecular mechanisms linking androgen dysregulation to hypertension seem to be related to increased visceral fat, promoting a chronic inflammatory state through different mechanisms. One proposed mechanism may involve the recruitment and over-activation of NF-kB where it may cause the production of inflammatory cytokines and other immune factors. Chronic inflammation and adipocyte dysfunction may alter endothelial function leading to hypertension. Both in men and in women, particularly in the postmenopausal period, low testosterone seems to be a major determinant of the increased prevalence of hypertension 13.
The role of androgens in women as it relates to heart disease cannot be understated. Studies show a positive association between low testosterone levels and severe atherosclerosis (heart disease) in postmenopausal women. Further, higher levels of androgens in postmenopausal women have a protective role in the development of atherosclerosis, and women in the ELITE trial who were on and stayed on estrogen had a 50% reduction in the progression rate of heart disease compared to women who were NOT on estrogen 14. Estrogen protects the heart from ischemic injury, and postmenopausal HT use is accompanied with reduced mortality risk after primary acute coronary syndrome. Authors concluded estrogen should be considered as a preventative strategy for reduction of bone loss, bone fractures, new onset diabetes mellitus, CHD and all-cause mortality 15.
9, Venetkoski, et.al., 2018; Salpeter, et.al., 2009; Sarrel, et.al., 2013; Mikkola, et.al., 2015; Hodis & Mack, 2018; Venetkoski, etal., 2018
10. Gururani , et.al., 2016; Malkin, ,et.al., 2004; Khaw, et.al., 2007
11. Chistiakov, et.al., 2018
12. Daka, et.al., 2015
13. Moretti, et.al., 2017

Neurological Disease
Hormone therapy, both estrogen and testosterone, plays an efficacious role in preventing neurodegenerative conditions. Estrogen can reduce the risk for
Alzheimer’s disease and minimize cognitive decline by protecting against B-amyloid induced degeneration 16. Estrogen is an immunomodulator and protects the brain from ischemic injury during and after stroke by activating several neuro-protective pathways in the brain. Following brain injury or ischemia, there is a rapid local production of estrogen, indicating that the hormone may be involved in an immediate physiological response to limit tissue damage 17.
Chronic Pain and Fibromyalgia
Chronic pain is a debilitating condition that is prevalent in society. Healthcare providers who utilize hormone optimization as a part of managing their chronic pain patients are forward thinking and understand opioid induced androgen deficiency, as well as the role sub optimal hormones play in the pain signaling threshold and pain transmission. Testosterone deficiency in chronic pain patients has now been recognized by many observers. Due to its critical biologic functions in pain control, testosterone testing and replacement is now recommended to be a mandatory component in the treatment of chronic pain. Numerous studies on both animals and human subjects have also demonstrated the potential effects of gonadal hormones, such as estrogens, on pain transmission. These effects most likely involve multiple neuroanatomical circuits as well as diverse neurochemical systems 18.
Given the plethora of data showing both estrogen and testosterone to down regulate pain signaling and be a mandatory component of pain management, estrogen and testosterone optimization in these patients is a vital aspect of their care.
14. Debing, et.al., 2007; Hodis, et.al., 2014
15. Mikkicola, et.al., 2015
16. Henderson, 2014
17. de Tassigny, 2017; Petrone, et.al., 2014; Petrone, et.al., 2015
18. Meganne, et.al., 2016; Tennant, F., & Lichota, 2010; Amandusson, & Blomqvist, 2013; Ghorbanpoor, et.al., 2014; White & Robinson, 2015
Final Thoughts
Treating thousands of patients, healthy and chronically ill alike, for over a decade with hormone optimization has afforded me a view many healthcare providers do not have. Countless healthcare providers, medical and nursing board appointees and lawmakers are still under the uninformed notion that hormone replacement is simply to curb symptoms of menopause transition in women, and sexual dysfunction in men. These notions could not be further from the truth, as partially demonstrated in this monograph. This writing is by no means an exhaustive list of the studies surrounding the importance of hormone homeostasis. There are literally thousands of studies that point to the crucial need for patients to remain on, or even start, a hormone therapy program, especially during times of extreme and excessive stress such as we are experiencing globally. For patients of hormone therapies who have been told your treatments are “not medically necessary” at this time, I urge you to respectfully disagree with your healthcare provider and/or find a provider who will help you.
For medical providers reading this work, I pray it has enlightened and reignited your sense of passion to provide the highest level of care for your patients.

Bibliography
1. Ahsan, M., Mallick, A. K., Singh, R., & Prasad, R. R. (2015). Assessment of menopausal symptoms during perimenopause and postmenopause in tertiary care hospital. Journal of Basic and Clinical Reproductive Sciences, 4(1), 14-19. 2. Amandusson, Å., & Blomqvist, A. (2013). Estrogenic influences in pain processing. Frontiers in neuroendocrinology, 34(4), 329-349. 3. Aminorroaya, A., Kelleher, S., Conway, A.J, Ly, L.P., & Handelsman, D.J. (2005). Adequacy of androgen replacement influences bone density response to testosterone in androgen deficient men. European Journal of Endocrinology, 152, 881-886. 4. Amory, J.K., Watts, N.B., Easley, K.A., Sutton, P.R., Anawalt, B.D., Matsumoto, A.M., Bremner, W.J., & Tenover, J.L. (2004). Exogenous Testosterone or Testosterone with Finasteride Increases Bone Mineral Density in Older Men with Low Serum Testosterone Levels. The Journal of Clinical Endocrinology, 89(2), 503-510. 5. Araujo, A.B., Dixon, J.M., Suarez, E.A., Murad, H.M., Guey, L.T. & Wittert, G.A. (2011). Clinical Review: Endogenous Testosterone and Mortality in Men: A Systematic review and Meta-Analysis. Journal of Clinical Endocrine Metabolism, 96(10), 1-13.
6. Bachmann, G. A. (1999). Androgen cotherapy in menopause: Evolving benefits and challenges. American Journal of Obstetrics and Gynecology, 180(3), S308-S311. 7. Barrett-Conner, E., Dam, T.T., Stone, K., Harrison, S.L., Redline, S. & Orwoll, E. (2008). The Association of Testosterone Levels with Overall Sleep Quality, Sleep Architecture, and Sleep-Disordered Breathing. Journal of Clinical Endocrine Metabolism, 93(7), 2602- 2609. 8. Beuachet, O. (2006). Testosterone and cognitive function: Current clinical evidence of a relationship. European Journal of Endocrinology, 155, 773-781. 9. Bialek, M., Zaremba, P., Borowicz, K.K., Czuczwar, S.J. (2004). Neuroprotective role of testosterone in the nervous system. Polish Journal of Pharmacology, 56, 509-518. 10. Boyanov, M.A., Boneva, Z., & Christov, V.G. (2003). Testosterone supplementation in men with type 2 diabetes, visceral obesity and partial androgen deficiency. The Aging Male, 6, 1-7. 11. Bromberger, J. T., Matthews, K. A., Schott, L. L., Brockwell, S., Avis, N. E., Kravitz, H. M., Randolph, John F.,,Jr. (2007). Depressive symptoms during the menopausal transition: The study of women’s health across the nation (SWAN). Journal of Affective Disorders,
103(1-3), 267-272. 12. Carnahan, R.M.& Perry, P.J. (2004). Depression in Aging Men: The role of testosterone. Aging Drugs, 21(6), 361-376. 13. Cherrier, M.M., Asthana, S., Plymate, S., Baker, L., Matsumoto, A.M., Peskind, E., Raskind, M.A., Brodkin, K., Bremner, W., Petrova, A., LaTendresse, S., & Craft, S. (2001). Testosterone supplementation improves spatial and verbal learning memory in healthy
older men. Neurology, 57, 80-88. 14. Chistiakov, D. A., Myasoedova, V. A., Melnichenko, A. A., Grechko, A. V., & Orekhov, A. N. (2018). Role of androgens in cardiovascular pathology. Vascular health and risk management, 14, 283. 15. Daka, B., Langer, R. D., Larsson, C. A., Rosén, T., Jansson, P. A., Råstam, L., & Lindblad, U. (2015). Low concentrations of serum testosterone predict acute myocardial infarction in men with type 2 diabetes mellitus. BMC endocrine disorders, 15(1), 35. 16. Davis, S. (1999). Androgen replacement in women: A commentary. Journal of Clinical
Endocrinology and Metabolism, 84(6), 1886-1891. Now More Than Ever: The Vital Role of Hormone Therapy in Managing Dis-ease 7 17. Davis, S. R., & Tran, J. (2001). Testosterone influences libido and well being in women. Trends in Endocrinology & Metabolism, 12(1), 33-37. 18. Davison, S.L., Bell. R.J., Gavrilescu, M., Searle, K., Maruff, P., Gogos, A., Rossell, S.L. Adams, J., Egan, G.F., & Davis, S.R. (2011). Testosterone improves verbal learning and memory in postmenopausal women: Results from a pilot study. Maturitas, 70, 307-311. 19. Debing, E., Peeters, E., Duquet, W., Poppe, K., Velkeniers, B., & Van den Brande, P. (2007). Endogenous sex hormone levels in postmenopausal women undergoing carotid artery endarterectomy. European journal of endocrinology, 156(6), 687-693. 20. de Tassigny, X. D. A. (2017). Outlook on the neuroprotective effect of estrogen. Neural regeneration research, 12(11), 1799. 21. Dimitrakakis, C. (2011). Androgens and Breast Cancer in Men and Women. Journal of Endocrinology Metabolism Clinics of North America, 40, 533-537. 22. Ðoković, D.,D., Jović, J.,J., Ðoković, J.,D., Knežević, M. Ž., Djukić-Dejanović, S., & RistićIgnjatović, D.,I. (2015). Effects of hormone replacement therapy on depressive and anxiety symptoms after oophorectomy. Medicinski Glasnik: Official Publication of the Medical Association of Zenica-Doboj Canton, Bosnia and Herzegovina, 12(1), 79-85.
23. Ebinger, M., Sievers, C., Ivan, D., Schneider, H. J., & Stalla, G. K. (2008). Is there a neuroendocrinological rationale for testosterone as a therapeutic option in depression? Journal of Psychopharmacology. 23(7), 841-853. 24. Freeman, E. W., Sammel, M. D., Liu, L., Gracia, C. R., Nelson, D. B., & Hollander, L. (2004). Hormones and menopausal status as predictors of depression in women in transition to menopause. Archives of General Psychiatry, 61(1), 62-70. 25. Frye, C. A., & Walf, A. A. (2009). Depression-like behavior of aged male and female mice is ameliorated with administration of testosterone or its metabolites. Physiology & behavior, 97(2), 266-269. 26. Gagliano-Jucá, T., Travison, T. G., Nguyen, P. L., Kantoff, P. W., Taplin, M. E., Kibel, A. S., .
& Huang, G. (2018). Effects of androgen deprivation therapy on pain perception, quality of life, and depression in men with prostate cancer. Journal of pain and symptom management, 55(2), 307-317. 27. Ghorbanpoor, S., Garcia-Segura, L. M., Haeri-Rohani, A., Khodagholi, F., & Jorjani, M. (2014). Aromatase inhibition exacerbates pain and reactive gliosis in the dorsal horn of the spinal cord of female rats caused by spinothalamic tract injury. Endocrinology, 155(11), 4341-4355 28. Glaser, R. & Dimitrakakis, C. (2013). Testosterone therapy in women: Myths andmisconceptions. Maturitas, 74(3), 230; 230-234; 234. 29. Glaser, R., Dimitrakakis, C., Trimble, N., & Martin, V. (2012). Testosterone pellet implants and migraine headaches: A pilot study. Maturitas, doi:10.1016/j.maturitas.2012.01.006. 30. Glaser, R., York, A. E., & Dimitrakakis, C. (2011). Beneficial effects of testosterone therapy in women measured by the validated menopause rating scale (MRS). Maturitas,
68(4), 355-361. 31. Goldstat, R., Briganti, E., Tran, J., Wolfe, R., & Davis, S. R. (2003). Transdermal testosterone therapy improves well-being, mood, and sexual function in premenopausal
women. Menopause, 10(5), 390-398. 32. Gururani, K., Jose, J., & George, P. V. (2016). Testosterone as a marker of coronary artery disease severity in middle aged males. Indian heart journal, 68, S16-S20.
Now More Than Ever: The Vital Role of Hormone Therapy in Managing Dis-ease 8 33. Gyllstrom, M. E., Schreiner, P. J., & Harlow, B. L. (2007). Perimenopause and depression:
strength of association, causal mechanisms and treatment recommendations. Best Practice & Research Clinical Obstetrics & Gynecology, 21(2), 275-292. 34. Hammond, J., Le., Q., Goodyer, C., Gelfand, M., Trifiro, M., & LeBlanc, A. (2001). Testosterone-mediated neuroprotection through androgen receptor in human primary neurons. Journal of Neurochemistry, 77, 1319-1326.
35. Henderson, V. W. (2014). Alzheimer’s disease: review of hormone therapy trials and implications for treatment and prevention after menopause. The Journal of steroid biochemistry and molecular biology, 142, 99-106. 36. Hodis, H. N., & Mack, W. J. (2018). Cardiovascular risk after withdrawal of hormone therapy. Menopause, 25(4), 365-367. 37. Hodis, H. N., Mack, W. J., Shoupe, D., Azen, S. P., Stanczyk, F. Z., Hwang-Levine, J., & Henderson, V. W. (2014). Testing the menopausal hormone therapy timing hypothesis: the Early versus Late Intervention Trial with Estradiol.
38. Hodosy, J., Zelmanová, D., Majzúnová, M., Filová, B., Malinová, M., Ostatníková, D., & Celec, P. (2012). The anxiolytic effect of testosterone in the rat is mediated via the androgen receptor. Pharmacology Biochemistry and Behavior, 102(2), 191-195. 39. Isodori, A.M., Gianetta, E., Greco, E.A., Gianfrilli, D., Bonifacio, V., Isidori, A., Lenzit, A., & Fabbri, A. (2005). Effects of testosterone on body composition, bone, metabolism, and serum lipid profile in middle aged men: A meta-analysis. Clinical Endocrinology, 63, 280- 293. 40. Jung, H. J., & Shin, H. S. (2016). Effect of testosterone replacement therapy on cognitive performance and depression in men with testosterone deficiency syndrome. The world journal of men’s health, 34(3), 194-199. 41. Khaw, K. T., Dowsett, M., Folkerd, E., Bingham, S., Wareham, N., Luben, R., … & Day, N. (2007). Endogenous testosterone and mortality due to all causes, cardiovascular disease, and cancer in men: European prospective investigation into cancer in Norfolk (EPIC-Norfolk) Prospective Population Study. Circulation, 116(23), 2694-2701.
42. Kotz, K., Alexander, J. L., & Dennerstein, L. (2006). Estrogen and androgen hormone therapy and well-being in surgically postmenopausal women. Journal of Women’s Health, 15(8), 898-908. 43. Lambrinoudaki, I., Bouziou, G., Armeni, E., Spyropoulou, A., Koundi, K., Rizos, D., & Dendrinos, S. (2015). Circulating androgens are associated with mood disturbances in young postmenopausal women. Climacteric, 18(2), 205-213. 44. Maartens, L., Knottnerus, J., & Pop, V. (2002). Menopausal transition and increased depressive symptomatology: A community based prospective study. Maturitas, 42(3), 195-200.
45. Malkin, C. J., Pugh, P. J., Morris, P. D., Kerry, K. E., Jones, R. D., Jones, T. H., & Channer, K. S. (2004). Testosterone replacement in hypogonadal men with angina improves ischaemic threshold and quality of life. Heart, 90(8), 871-876 46. McHenry, J., Carrier, N., Hull, E., & Kabbaj, M. (2014). Sex differences in anxiety and depression: Role of testosterone. Frontiers in Neuroendocrinology, 35(1), 42-57. 47. Meggane Melchior, Pierrick Poisbeau, Isabelle Gaumond, Serge Marchand: Insights into the mechanisms and the emergence of sex-differences in pain. Neuroscience, Volume
338, 2016, pp. 63-80 48. Mikkola, T. S., Tuomikoski, P., Lyytinen, H., Korhonen, P., Hoti, F., Vattulainen, P.,&Ylikorkala, O. (2015). Increased cardiovascular mortality risk in women discontinuing
Now More Than Ever: The Vital Role of Hormone Therapy in Managing Dis-ease 9 postmenopausal hormone therapy. The Journal of Clinical Endocrinology & Metabolism, 100(12), 4588-4594. 49. Mikkola, T. S., Tuomikoski, P., Lyytinen, H., Korhonen, P., Hoti, F., Vattulainen, P., … & Ylikorkala, O. (2015). Estradiol-based postmenopausal hormone therapy and risk of cardiovascular and all-cause mortality. Menopause, 22(9), 976-983. 50. Miller, K. K., Perlis, R. H., Papakostas, G. I., Mischoulon, D., Iosifescu, D. V., Brick, D. J., & Fava, M. (2009). Low-dose transdermal testosterone augmentation therapy improves depression severity in women. CNS spectrums, 14(12), 688-694. 51. Miller, K. K., Wexler, T. L., Zha, A. M., Lawson, E. A., Meenaghan, E. M., Misra, M., & Klibanski, A. (2007). Androgen deficiency: association with increased anxiety and depression symptom severity in anorexia nervosa. The Journal of clinical psychiatry, 68(6), 959-965. 52. Montgomery, J. C., Appleby, L., Brincat, M., Versi, E., Tapp, A., Fenwick, P. B., & Studd, J. W. (1987). Effect of oestrogen and testosterone implants on psychological disorders in the climacteric. Lancet (London, England), 1(8528), 297-299. 53. Moretti, C., Lanzolla, G., Moretti, M., Gnessi, L., & Carmina, E. (2017). Androgens and hypertension in men and women: a unifying view. Current hypertension reports, 19(5), 44. 54. Nappi, R.E. & Lachowsky, M. (2009). Menopause and sexuality: Prevalence of symptoms and impact on quality of life. Maturitas, 63, 138-141. 55. Okun, M.S., Walter, B.L., McDonald, W.M., Tenover, J.L., green, J., Juncos, J.L., &
DeLong, M.R. (2002). Beneficial Effects of Testosterone Replacement for the Non-motor Symptoms of Parkinson’s Disease. Archives of Neurology, 59, 1750-1753.
56. Osborne, D. M., Edinger, K., & Frye, C. A. (2009). Chronic administration of androgens with actions at estrogen receptor beta have anti-anxiety and cognitive-enhancing effects
in male rats. Age, 31(3), 191-198. 57. Panay, N., & Fenton, A. (2009). The role of testosterone in women. Climacteric, 12(3), 185-187. 58. Panzer, C., & Guay, A. (2009). Testosterone replacement therapy in naturally and surgically menopausal women. The Journal of Sexual Medicine, 6(1), 8-18. doi:10.1111/j.1743-6109.2008.01128.x 59. Petrone, A. B., Simpkins, J. W., & Barr, T. L. (2014). 17β-estradiol and inflammation: implications for ischemic stroke. Aging and disease, 5(5), 340. 60. Petrone, A. B., Rudy, C. C., Barr, T. L., Simpkins, J. W., & Reed, M. N. (2015). Neuroprotective effects of estrogen following neural injury. In Estrogen Effects on Traumatic Brain Injury (pp. 91-111). 61. Pike, C., Carroll, J.C., Rosario, E.R., & Barron, A.M. (2009). Protective actions of sex steroid hormones in Alzheimer’s disease. Frontiers in Neuroendocrinology, 30, 239-258. 62. Rohr, U. D. (2002). The impact of testosterone imbalance on depression and women’s health. Maturitas, 41 Suppl 1, S25-S46. 63. Sands, R. & Studd, J. (1995). Exogenous Androgens in Postmenopausal Women. The American Journal of Medicine, 98(1A), 76-79. 64. Salpeter, S. R., Cheng, J., Thabane, L., Buckley, N. S., & Salpeter, E. E. (2009). Bayesian
meta-analysis of hormone therapy and mortality in younger postmenopausal women. The American journal of medicine, 122(11), 1016-1022. 65. Sarrel, P. M., Njike, V. Y., Vinante, V., & Katz, D. L. (2013). The mortality toll of estrogen avoidance: an analysis of excess deaths among hysterectomized women aged 50 to 59 years. American journal of public health, 103(9), 1583-1588. Now More Than Ever: The Vital Role of Hormone Therapy in Managing Dis-ease 10 66. Schutter, D. J., Peper, J. S., Koppeschaar, H. P., Kahn, R. S., & van Honk, J. (2005). Administration of testosterone increases functional connectivity in a cortico-cortical depression circuit. The Journal of neuropsychiatry and clinical neurosciences, 17(3), 372- 377. 67. Soares, C. N., Poitras, J. R., & Prouty, J. (2003). Effect of reproductive hormones and selective estrogen receptor modulators on mood during menopause. Drugs & Aging, 20(2), 85-100. 68. Studd, J., & Panay, N. (2004). Hormones and depression in women. Climacteric: The
Journal of the International Menopause Society, 7(4), 338-346. 69. Tennant, F., & Lichota, L. (2010). Testosterone replacement in chronic pain patients. Pract Pain Manag, 10, 12-15. 70. Utian, W. H. (1994). Ovarian function, therapy-oriented definition of menopause and climacteric. Experimental Gerontology, 29(3), 245-251. 71. Vanderschueren, D., Vandenput, L., Boonen, S., Lindberg, M.K., Bouillon, R., & Ohlsson, C. (2004). Androgens and Bone. Endocrine Reviews, 25(3), 389-425. 72. Venetkoski, M., Savolainen-Peltonen, H., Rahkola-Soisalo, P., Hoti, F., Vattulainen, P., Gissler, M., … & Mikkola, T. S. (2018). Increased cardiac and stroke death risk in the first year after discontinuation of postmenopausal hormone therapy. Menopause, 25(4), 375-379.
73. White, H. D., & Robinson, T. D. (2015). A novel use for testosterone to treat central sensitization of chronic pain in fibromyalgia patients. International Immunopharmacology, 27(2), 244-248. 74. Woods, N. F., & Mitchell, E. S. (2005). Symptoms during the peri-menopause: prevalence, severity, trajectory, and significance in women’s lives. The American journal of medicine, 118(12), 14-24.
75. Wuttke, W., Seidlova-Wuttke, D., & Gorkow, C. (2003). The Cimicifuga preparation BNO 1055 vs. conjugated estrogens in a double-blind placebo-controlled study: effects
on menopause symptoms and bone markers. Maturitas, 44, S67-S77. 76. Zarrouf, F. A., Artz, S., Griffith, J., Sirbu, C., & Kommor, M. (2009). Testosterone and depression: systematic review and meta-analysis. Journal of Psychiatric Practice, 15(4), 289-305.
Subscribe Today!
Be the first to get latest updates and
exclusive content straight to your email inbox.
We do not spam. You can unsubscribe anytime.






